Preventing Osteoporosis The Natural Way
Preventing Osteoporosis The Natural Way
The functional medicine approach to osteoporosis is to look at the body’s interconnected systems to understand the causes of deteriorating bone health, build bone strength and improve overall health.
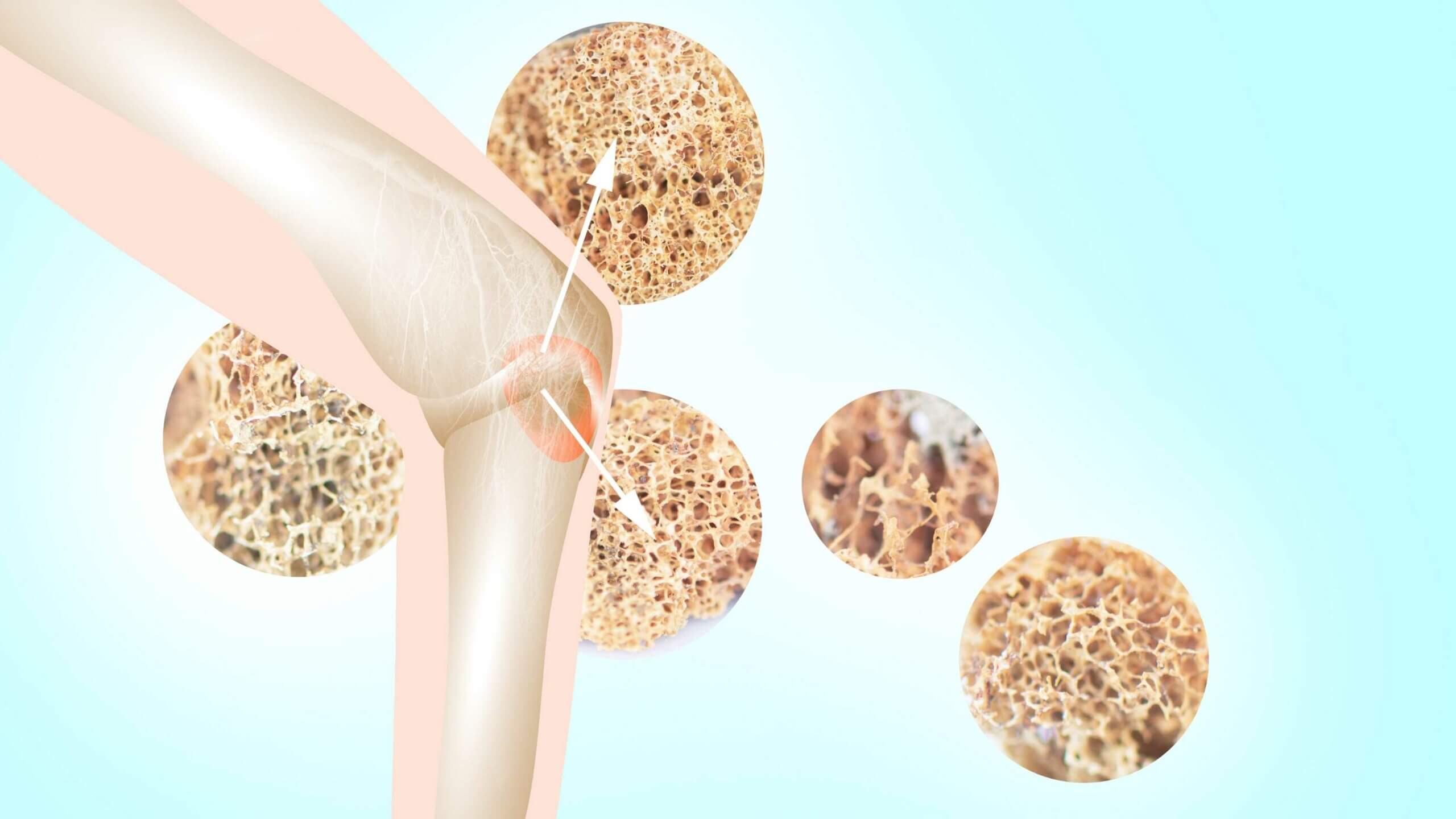
Osteoporosis means ‘porous bones’. It is a condition where bones become thin, weak and fragile and even a minor bump or accident can cause a bone to break, especially in the hip, wrist and spine.
An estimated 924,000 Australians have osteoporosis, representing 3.8% of the population. It is often underdiagnosed but can be catastrophic in terms of quality of life and can result in chronic pain, disability, loss of independence and premature death. [1]
What is osteoporosis?
Bone is living tissue that is constantly being broken down and replaced. Osteoporosis occurs when the creation of new bone doesn’t keep up with the loss of old bone.
Osteopenia is a condition when bone mineral density is lower than normal but not low enough to be classified as osteoporosis.
Your body continuously breaks down and rebuilds bone. Before you reach your 30s, you make more bone than you break down so bone density increases. After your mid-30s, your body continues to make new bone, but at a slower speed so you can lose more bone than you make.
There are often no symptoms of osteoporosis. Reported numbers of people with osteoporosis is often lower than reality as many people don’t know they have the condition until a fracture occurs and further investigation is conducted.
Once your bones have been weakened by osteoporosis, you might have signs and symptoms that include:
- Back pain, caused by a fractured or collapsed vertebra
- Loss of height over time
- A stooped posture
- A bone that breaks much more easily than expected [2]
What causes osteoporosis?
The skeleton is a metabolically active organ that is continually changing throughout our lives due to two cells – osteoblasts and osteoclasts.
Osteoblasts are cells that instruct the body to build bones. They deposit new collagen that will become strong bone filled with minerals.
Osteoclasts are cells that instruct the body to break down bone, ingest the resulting fragments and release the stored minerals into the bloodstream.
Osteocytes live in the bone and are the supervisor cells that oversee the process.
When osteoblasts and osteoclasts are functioning as they should, our bones are healthy and strong. When they are uncoordinated due to dysfunctions in other systems in the body, osteoclast production outpaces osteoblast production and bone is broken down faster than it is being built. [3]
Risk factors for osteoporosis
The amount of calcium and other supportive minerals are in the bone determine your bone strength and density and there are many factors that influence the ability to maintain bone mineralization.
Risk factors associated with the development of osteoporosis include:
Age – Older age groups also tend to be affected. The proportion of women with osteoporosis increases with age, with those 75 and over being most affected. [4]
Sex – Osteoporosis is more common in women than men. In 2017–18, 29% of women aged 75 and over had osteoporosis compared with 10% of men. [5]
During menopause women experience bone loss due to the relationship between estrogen and calcitonin, the hormone in charge of regulating blood calcium levels. After a woman’s menstrual cycle stops, the primary circulating estrogen in the body becomes estrone, which is ten times weaker than estradiol. So estrogen levels drop with menopause and also become weaker forms of estrogen. This combination of factors will decrease levels of calcitonin and, in effect, decrease bone mineralization and density. [6]
Family history of the condition – Many studies have demonstrated the link between genetics and osteoporosis. One 2019 study demonstrated the presence of osteoporosis in close relatives (usually the mother) and the existence of previous fractures are significant risk factors for the occurrence of osteoporosis. [7] It is recommended that if your parents have osteoporosis, you get tested and commence preventative measures.
Low vitamin D levels – Vitamin D stimulates the absorption of calcium from the gut, decreases bone turnover and increases bone mineral density. Vitamin D deficiency causes secondary hyperparathyroidism and bone loss, leading to osteoporosis and fractures, mineralization defects, which may lead to osteomalacia in the long term, and muscle weakness, causing falls and fractures. [8]
Supplementing with Vitamin D if your levels are low is key to reducing your risk of developing osteoporosis.
Diet low in nutrients and calcium – ensuring that you obtain the highest level of nutrients from your food is key to preventing and treating osteoporosis. Eat brightly coloured, fresh vegetables that will ensure you receive a wide range of vitamins and minerals. Milk and other dairy products have traditionally been the solution for improving calcium levels although calcium from dairy products is not always easily absorbed. There are many other calcium-rich alternatives to dairy including chia seeds, almonds, pink salmon, dried figs, tofu, white beans, sunflower seeds, broccoli rabe, sesame seeds, sweet potatoes, oranges, butternut squash, arugula (rocket), oatmeal, soybeans and turnips.
Chronic inflammation – the immune system is always turned on, leading to an unbalanced system. The bone marrow is where your immune system cells are created so when the system is unbalanced system, your bones will suffer.
Diseases associated with gut inflammation, such as Crohn’s disease, have been shown to impair calcium absorption. The inflammation that is central to rheumatoid arthritis is a risk factor for osteoporosis in itself. Data shows that both active inflammation in the bone, and systemic inflammation, lead to an increased risk of osteoporosis and osteoporotic fractures. [9]
Smoking – Studies have shown a direct relationship between tobacco use and decreased bone density although this relationship is complicated as its difficult to determine if a decrease in bone density is due to smoking itself or to other risk factors common among people who smoke.
The elevation of stress hormones – The physiological factors of stress involve endocrinological changes, such as increased glucocorticoids, prolactin, leptin and parathyroid hormone levels and reduced gonadal hormones. Low-grade inflammation and hyperactivation of the sympathetic nervous system during psychological stress are also physiological changes detrimental to bone health. [10]
In addition, when stress becomes chronic, our diets cannot replace the calcium depletion fast enough, so our bones are constantly being leached of calcium, leading to potentially more porous bones, brittle bones and osteoporosis.
Excessive alcohol consumption – Studies demonstrate that chronic, heavy alcohol consumption compromises bone health and increases the risk of osteoporosis. In particular, heavy alcohol use decreases bone density and weakens bones’ mechanical properties. [11]
Physical inactivity – one of the most important things you can do to improve bone health is to exercise to strengthen bone, build muscle and improve balance to prevent falls. Strength and resistance training is idea.
Long-term corticosteroid use – Steroids have major effects on how the body uses calcium and vitamin D to build bones. Steroids can lead to bone loss, osteoporosis, and broken bones.
Other conditions – osteoporosis can be caused by diseases such as autoimmune disease, cancer, cystic fibrosis, diabetes, MS and Parkinson’s disease.
Treating osteoporosis, the natural way
- Optimise vitamin D. The recommended intake of Vitamin D is 800 to 1000 international units (IU) of vitamin D3 per day for adults over age 50.
- Optimise vitamin K. Vitamin K has long been known to be important for blood clotting. In fact, its name comes from the German word koagulation. Research has suggested that Vitamin K also plays a key role in controlling bone metabolism because it’s essential for synthesizing osteocalcin, an important protein for maintaining bone strength. [12]
- Supplement with alpha lipoic acid. ALA has antioxidant properties and can reduce oxidative stress as well as inflammation which slows osteoclastic bone-resorbing activity.
- Supplement with berberine. Research suggests that berberine may lower osteoclast activity and boost osteoblast activity.
- Eat protein. Protein is the basis for bone and collagen so make sure you get enough of this macronutrient. [13] When your body’s collagen production decreases, your bones weaken, making them more susceptible to fracture. Studies show that taking collagen peptides may be helpful in treating and preventing osteoporosis.
- Eat an anti-inflammatory diet. Eat an anti-inflammatory diet with plenty of omega-3 fats and reduce your consumption of gluten and sugar.
- Get plenty of sleep. Melatonin affects the actions of osteoblasts and osteoclasts and interacts with other hormones like estrogen to augment bone remodelling. And it also functions as a really potent antioxidant which protects bone cells from oxidative stress and inflammation. Limit your exposure to artificial light at night, getting some exposure to bright sunlight during the day and get at least 7 to 8 hours at least of quality sleep per night to boost melatonin production. [14]
How we can help
Bone health can be improved through the right tailored diet, strength-building exercise and supplementation. By improving your exercise regime and eating more healthily, you’ll not only create healthier bones, but you’ll also boost your overall health.
A functional medicine approach to osteoporosis focusses on prevention and the root causes of osteoporosis, many of which are inextricably linked to other systems in the body. By treating the body holistically, our functional medicine health practitioners at Advanced Functional Medicine can look for underlying causes, conduct rigorous testing and ultimately, find effective methods to assist with the health of your bones.
Contact us to find out more.




